Many circumstances, such as in-vitro fertilization, can impair the success of infertility therapies (IVF). A woman may have a poor response to ovarian stimulation, and create eggs that do not fertilize or produce chromosomally defective embryos. Her uterine lining might not be thick enough to enable implantation, or there could be another reason for the failure, such as oocyte/embryo injury during unfreezing or transfer. You should pgd vs pgs testing to get information of condition.
The egg retrieval and embryo transfer procedures can also go wrong—sometimes because of the doctor’s inexperience, but more often due to uterine contractility. However, of all of these criteria, chromosomal aberration is the one that determines the majority of instances’ success.
The success of most infertility therapies is based on the ovulation of many eggs at the same time. At least one of those eggs will be fertilized, implanted in the uterine lining, and develop into a healthy fetus, according to the hope. A substantial percentage of a woman’s eggs will be of poor quality and have a chromosomal defect if she is over 35. (e.g., a trisomy or monosomy).
Chemical Pregnancy
A chemical pregnancy or a miscarriage later in the pregnancy is virtually invariably the result of such anomalies. How can they be identified and removed as a contributing factor? By choosing IVF with chromosome preimplantation genetic screening (PGS).
Although PGS does not prevent chromosomal abnormalities, it improves one’s chances of becoming pregnant by detecting aneuploids (cell division errors that result in a chromosome number that is not an exact multiple of the haploid number) and allowing the doctor and patient to transfer only healthy embryos. With chromosomal abnormalities effectively eliminated from the list of possible causes of a failed pregnancy, a woman’s chances of a successful pregnancy increase to around 85%.
PGS works by taking a sample of an egg or embryo and counting the chromosomes of one or more cells. In addition to XX (female) or XY (male), normal cells have 22 pairs of chromosomes for a total of 46 chromosomes. From the mother’s egg and the father’s sperm, a newborn receives one of each pair. However, for unexplained reasons, an egg or sperm may contain too many or too few chromosomes, endangering the embryo’s viability.
Even though such chromosomal abnormalities can be found both naturally and with assisted reproduction methods, they can be detected before pregnancy begins with IVF thanks to PGS, and the decision to not implant these faulty embryos can be made.
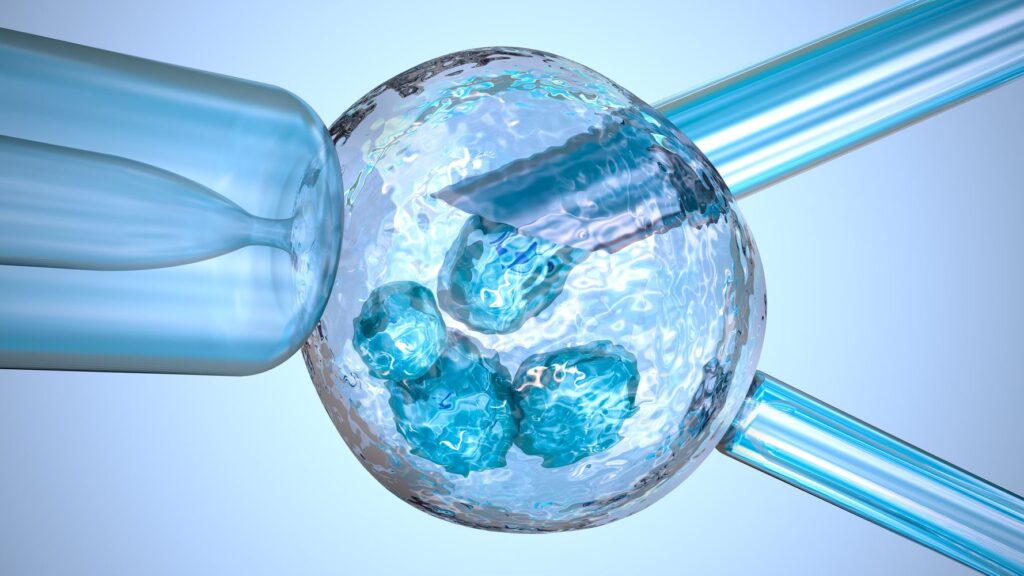
An embryologist collects a tiny sample of the egg or embryo for analysis using a small needle during a PGS.
Then One of Three Ways Can Be Used:
- Test the polar body on the outside of the egg
- Test a blastomere (one cell) from a third-day-of-development egg, or
- Test a trophectoderm (many cells) from a fifth-day-of-development embryo.
The egg/embryo is either returned to the incubator (to continue growing) or frozen for future use after the chromosomes have been counted.
What Is Pgd Testing for Gender Selection and How Does It Work?
Preimplantation genetic diagnosis, or PGD for short, is a technique for detecting genetic problems in embryos generated through in vitro fertilization or other forms of assisted reproduction technology. The method can also be used to determine a person’s gender. The operation will be performed by a specialist who will evaluate the genetic makeup of the embryos developed to look for genetic abnormalities as well as the couple’s desired gender.
The procedure begins with the mother’s eggs being extracted, followed by the father’s sperm being used to generate embryos. The sperm is used to fertilize the eggs in a laboratory, and numerous embryos will have developed after around three days. The embryos’ genetic makeup will subsequently be screened and examined by the specialist. They’ll check for genetic abnormalities and malformations, as well as the embryo’s gender.
Healthy embryos of the chosen gender will be taken and implanted in the mother’s uterus by the specialist. The embryos may then implant in the uterine wall and mature, leading to birth as it would if conception had occurred spontaneously. Couples have the option of freezing additional healthy embryos for later use.
Peoples considering gender selection should be aware that there are ethical difficulties with the procedure, particularly when it is undertaken for social or emotional reasons rather than to avoid a genetic condition. Those who are interested in the procedure should speak with an expert to learn more about it. During a consultation, the couple may have ethical issues as they examine if the process is right for them.
According to reports, there is a 98 percent chance that the embryo will not have a genetic problem and a 99 percent chance that the embryo will be of the chosen gender using this technique. False-positive or false-negative test findings are among the risks associated with PGD. There may be chromosomal discrepancies from cell to cell, which means the biopsied cell may not be indicative of the embryo’s other cells.
Cost
The cost of PGD can be fairly costly, and many insurance companies do not cover it. In vitro fertilization (IVF) costs may rise by roughly $3,500 as a result of the operation, though this may vary. Peoples should speak with a professional at the International Fertility Group where they plan to receive treatment or undergo testing about costs. You must evaluate the service and care provided once the surgery is completed.
A preimplantation genetic diagnosis was suggested by my doctor. This was a relatively new surgery at the time, and the physicians thought it was revolutionary, but I have to admit that I was not entirely comfortable with it. PGD, according to my doctor, would prevent me from having a child with a genetic problem. I tried but failed to obtain further information from other doctors and researchers. At the time, internet access was limited, and little information on PGD was available in traditional media or libraries.
Final Thought
PGS testing does not ensure that a pregnancy will occur or that the pregnancy will result in a healthy baby free of genetic abnormalities. The screening has some limitations, including the fact that it does not look for mitochondrial dysfunction or the likelihood of an inherited genetic condition. Preimplantation genetic diagnosis (PGD) is a new way of testing for specific mutations that is only requested if the couple has been identified to have a high risk of producing a child with a genetic disorder after genetic testing of the future parents.